Canuck Place nurses pave the way for Pediatric Palliative Care (PPC)
This week is National Nursing Week — a very important week at Canuck Place. Canuck Place nurses are compassionate, and resilient, and provide exceptional complex care to the children and families on our program.
National Nursing Week theme this year is “Our Nurses. Our Future”. Canuck Place nurses play many roles in a family’s journey. Our nurse practitioners, clinical nurse specialists, and nurses are highly trained, specialized professionals in PPC nursing. They provide assessment, pain and symptom management, care planning, and follow-up support for children living with life-limiting illnesses and the families who love them.
Canuck Place nurses also share their knowledge and expertise with healthcare providers and communities worldwide.
We sat down with Canuck Place Registered Nurse, Melanie Hameluck to learn more about her role at Canuck Place and how she helps train nurses around the world in PPC.

-
Tell us about yourself and your role at Canuck Place?
I am a registered nurse at Canuck Place and BC Children’s Hospital Oncology, Hematology, and Bone Marrow Transplant program. I have been at Canuck Place for six years now, working 12-hour day and night shifts caring for the families who are in the Vancouver hospice. The care our nursing team provides ranges from respite care to symptom management and end-of-life care. We also help manage the 24/7 Clinical Care Line available to every family on our program.
Caring for children and families is an absolute honor and privilege. I am often in awe of the resilience and strength I witness in the children and families I care for. I wish we lived in a world where families didn’t have to access oncology or palliative care, but unfortunately, that isn’t the case. PPC is about making a very difficult time a little easier on families. We walk with families through uncertainty, hardship, memory-making, major changes, difficult decision-making, hope, and loss. Some days we are playing with children and families in our garden, some days we are on an outing with the recreation therapy team providing care while a child is adventuring, and other days we are helping a child stay comfortable during their last breaths.
I have gone to the beach with families so their child can touch the ocean for the first time. I have taken a patient to the nail salon so she could feel like herself again, and I have administered pain meds through IV lines during NHL games so kids can stay focused on cheering for goals. Without a member of our nursing team present, our families are less likely to do things that might give them meaning during their last moments with their child because they are worried about their child’s comfort or stability. A nurse offers the safety net they need to get out and create memories while there is still time. Seeing our healthcare team make a positive impact on a family and witnessing the love they share is why I do this work.
2. How does being a PPC nurse in your opinion differ from other types of nursing roles?
At Canuck Place we often care for children at the end of their lives, but our healthcare team is so much more focused on helping a child live as much as they can and as comfortably as they can while the time is uncertain. As a PPC nurse, I often tell people I witness so much love. PPC is so unique. I truly believe it is the most family-centered, holistic approach to care you can find in a healthcare setting. When a person is admitted to the hospital, their worlds are instantly turned upside down. They now have to follow the timing, and rules, and adapt to the busy and often noisy environment of the hospital. PPC means giving as much control to a family and helping their world spin a little less. We meet families where they are at, meaning we allow them to tell us what they need and guide care. Families help us create care plans, decide the timing of medication and care, tell us how much nursing support they desire, and how they want to spend their days. I absolutely love this aspect of PPC because we are helping families and children spend time the way that suits them best and giving control back to families that have often had it taken away from them in other healthcare settings.
What often sets Canuck Place apart from the hospital is the amount of recreation and creativity we can put into care and what we can make happen for families. I am so grateful for our recreation team and what they advocate for and arrange no matter how much notice they have. I once cared for a young girl who was near the end of her life. Her father shared with us that one of the things he was grieving was the inability to one day be able to walk his daughter down the aisle. Hearing this, with the family’s wish, the recreation team arranged a photographer, music, decorations, and a beautiful veil. Then we picked a day for the family to honor their little girl. We spent the day in the garden with the whole family dressed up beautifully. I provided the infusions and medications she needed to remain comfortable throughout the day. We played a meaningful song while the father carried his sweet girl through the garden and “down the aisle” in a beautiful white unicorn dress, flower crown, and veil. She felt like a princess. Being present during these moments and having families trust us to care for their children on days like this is beyond special. The amount of love that I witnessed is immeasurable.
3. Canuck Place prides itself on knowledge sharing and innovation, can you share with us details about your recent trip to Nepal and India?
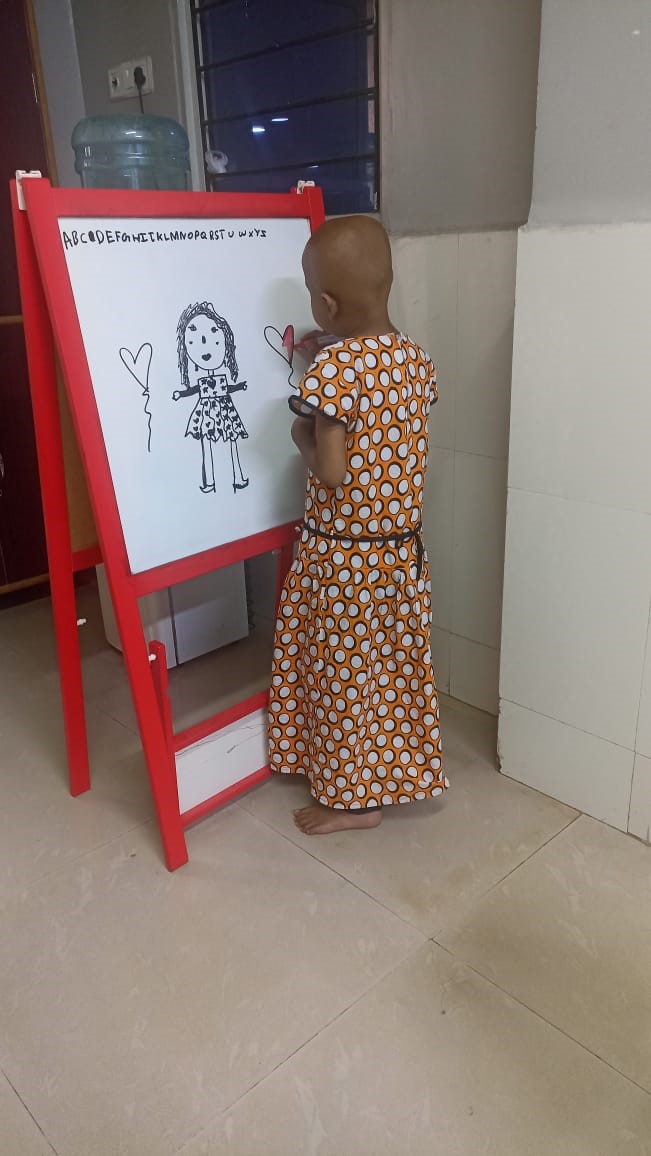
I recently had the opportunity to go to both India and Nepal to teach and advocate for PPC. I was accompanied by two other members of the Canuck Place team; Nurse Practitioner, Camara Van Breemen and Dr. Natasha Datoo. Our team worked with healthcare professionals both interested in and providing PPC in hospices, hospitals, and rural communities. Furthermore, in areas where palliative care is less known or discussed, we were able to introduce the topic and discuss the importance of it. We provided hands-on mentorship, lectures, and some smaller teaching sessions to nurses and doctors. I discussed topics such as comfort care with oncology patients, symptom management, play therapy during procedures, various oncology topics, ChildKind approach to care and pain relief, assessing/treating pain, comfort holds, non-pharmacological pain relief, and having difficult conversations with children and families.

a. What was the trip for/what was the organization?
I volunteer for the Sunflower Children’s Network which is Two Worlds Cancer’s Collaboration’s pediatric care initiative. Approximately 80% of young people in Canada survive cancer and serious illnesses. As much as I believe this number still isn’t high enough, the devastating truth is that 80% of young people in the countries we volunteer in will die from serious illness or cancer.
Two Worlds Cancer Collaboration’s aim is to reduce the burden of serious illnesses on families in resource-constrained countries. The Canadian-based charity supports programs in India, Nepal, Sri Lanka, Bangladesh, and the Philippines. The goal of the Sunflower Children’s Network is to develop and expand children’s healthcare centers and access to healthcare providers with palliative care specialization who can care for children with serious illnesses. We do this by providing education and mentorship which supports local healthcare providers to develop equitable and accessible healthcare programs that improve disease prevention, diagnosis, curative treatment, and palliative and end-of-life care. Two Worlds Cancer Collaboration volunteers teach on online video platforms as well as take trips to mentor, advocate, and teach in person.
When we visit our colleagues and join them at the bedside or homes of the children they care for, we witness the challenges they face in providing care to children, and we can truly understand what resources are available to them.
Understanding these aspects is incredibly important when it comes to building sustainable practices. And we get to build stronger connections with the nurses and physicians who share the same passion for helping children and families through serious illnesses as we do at Canuck Place.
b. What skills gained from your work at Canuck Place did you share?
Canuck Place has taught me so much. I am so lucky to work with some of the most knowledgeable, experienced, and passionate people in PPC. I love my team. From my days as a junior nurse witnessing experienced nurses navigate through compassionate conversations with families, to having the physicians discuss plans of care, medications, and rationales, Canuck Place has made me the nurse I am today. You learn on the job every day in this line of work. I still believe I have so much to learn and so many ways I can grow and become better as a PPC nurse, but the knowledge I have gained is so valuable. Whenever I have faced challenges, whether it be how to tell a family certain news or what medication I can give to help a child with their current symptoms, I am surrounded by and have access to some of the leading providers of palliative care. You can’t just read a textbook on PPC. When I am volunteering, I am able to share the experiences I have had as a nurse and what I have witnessed be successful or not successful. Continuing to connect with other practitioners overseas who are in more isolated settings is so important. When they share with us stories or case studies they are currently experiencing, we are able to offer our experience and guide each other through decision-making.
-
How do you think this knowledge-sharing experience emulates how Canuck Place is a leader in PPC nursing?
Canuck Place doesn’t just care about the children who are in house at Canuck Place. We care about the children in the community needing PPC, the children in the hospital who need PPC, and the children in other countries who can’t access PPC. Many of us work in various settings and are consistently trying to bring a bit of a PPC lens with us wherever we work. This means being able to carry and hold uncertainty and difficult conversations with families, recognizing physical and emotional pain and comfort in children, and advocating for families to be heard and honored.
5. How do you hope to continue your work in PPC knowledge sharing?
First of all, I am still constantly learning new things every day at work. I am faced with new situations, new solutions, and new conversations. I love that working in this field pushes you to continue to be better and continue to learn so you can give the best care possible. I am always learning from the families I work with, my colleagues at Canuck Place and BC Children’s Hospital, and my colleagues I volunteer with at Two Worlds Cancer Collaboration.
Personally, I want to continue to be involved in PPC on a global health capacity. I will continue to teach and connect with members of other communities to support the growth of palliative care. I also think sharing knowledge in other settings such as the hospital has always been something I find rewarding even when it is difficult at times. For example, when families are introduced to our team or hear about our hospice, they often are understandably overwhelmed or skeptical about what this means for their child. Because I am already working with those families in the hospital, I can be a tool for them when they have questions or concerns. I am able to offer reassurance that our team is just simply another tool to help their child live as well as possible for as long as possible. When I am able to help families navigate the next steps or just provide space for a conversation, I feel like my presence and experience at Canuck Place can make a difference.
6. What do you hope for in the evolution of PPC nursing care?
Ultimately, I want to see equity improve and for more families to have access to PPC worldwide. It breaks my heart that where you are born affects the ability of children to have access to comfort care. PPC has expanded so much over the past few decades. More and more families who need it are accessing palliative care every year because of an increase in both specialized practitioners, new facilities, and the general growth of knowledge in healthcare workers. I look forward to seeing how much it grows and expands throughout my career. Furthermore, I am really hoping I can help with that.

All photographs were taken by Harsha Vadlamani and Narendra Shrestha, Two Worlds Cancer.